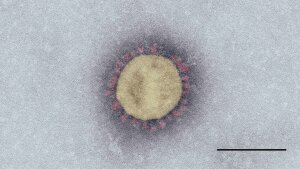
Electron micrograph of »SARS-CoV-2«. Scale: 100 nm.
Picture: Tobias Hoffmann, Michael Laue/RKI»SARS-CoV-2« (severe acute respiratory syndrome coronavirus 2) first emerged in China at the end of 2019. The pathogen, which is often referred to simply as the »novel coronavirus«, is closely related to the SARS virus (»SARS-CoV-1«), which triggered a pandemic in 2002/2003. It’s also closely related to the »MERS-CoV« virus, which has mainly been spreading on the Arabian Peninsula since 2012, causing equally severe respiratory diseases.
The spherical »SARS-CoV-2« virus particles are just under 100 nanometres on average. Their surface is covered in spikes measuring around 10 nanometres, which is how the virus gets its name (»corona« means crown). The genome of »SARS-CoV-2« and other coronaviruses consists of single-stranded RNA, containing almost 30,000 nucleotides (chain building blocks) that encode information on the construction of ten proteins.
Similar to other research teams around the world, scientists at Jena University Hospital have been forming interdisciplinary networks and carrying out intensive research into SARS-CoV-2 and the disease it causes, COVID-19, since the beginning of the year. Here are just some of the projects in Jena:
Sequencing of SARS-CoV-2 patient samples
A look into the coronavirus genome
To determine whether someone has become infected with SARS-CoV-2, a throat or nasal swab is taken and the viral genetic material in it is replicated. Subsequently, defined gene segments specific for the virus can be identified and it can be determined with certainty whether or not virus particles are present in the patient sample.
But not all coronaviruses are the same. As with higher organisms, there are variations in the genome of viruses. Moreover, their genetic information changes over time due to mutations. In order to track down such genetic changes in SARS-CoV-2, individual virus genomes, for example from patient samples, are now being completely sequenced. In other words, the sequencing is not limited to the segments necessary for identification, but the sequence of the entire genetic information is decoded. »The aim of such sequence analyses is to examine similarities in the structure of coronaviruses and draw conclusions about their origin«, says Dr Oliwia Makarewicz. The head of the research laboratory at the Institute of Infectious Diseases and Infection Control and her team are members of the national NFDI4MicrobiotaExternal link consortium, which is sequencing isolated SARS-CoV-2 genomes in Germany. Since March, the researchers have been regularly working with bioinformatician Prof. Manja Marz and her team from the European Virus Bioinformatics CentreExternal link at the University of Jena to analyse samples collected from COVID-19 patients at Jena University Hospital. They’ve been using the MinION system, a small mobile sequencing device that is hardly bigger than a USB stick and can be connected to a laptop or PC.
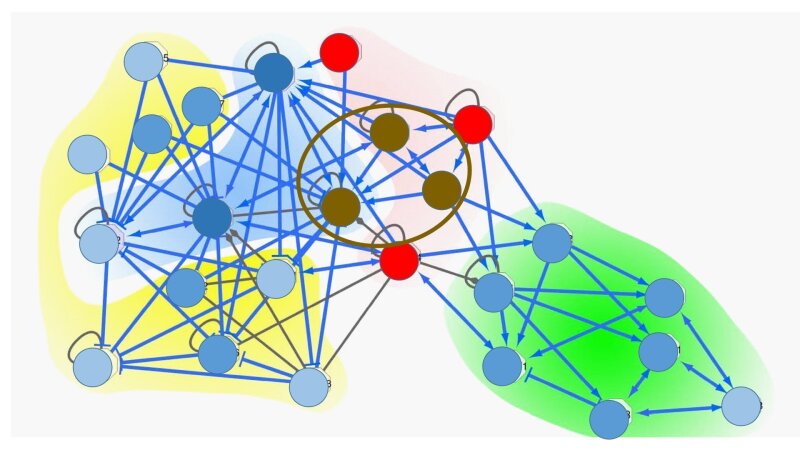
Global occurrence of the B.1.1. SARS-CoV-2 lineage. This lineage is mainly found in Europe.
Illustration: Erstellt mit https://pangolin.cog-uk.io/ und https://microreact.org/ am 14.07.2020»We’ve sequenced a little over 50 SARS-CoV-2 samples since March«, reports Dr Christian Brandt from the research team. Most of the samples have been taken directly at Jena University Hospital, but the team has also been working with samples from other hospitals in Thuringia and outpatient laboratories from all over Germany. All the samples examined so far have contained viruses from the B.1 lineage and the B.1.1 sub-class. The B.1.1 lineage has been found almost all over the world, but mainly in Europe (see map). Almost 100 SARS-CoV-2 lineages have been described around the world. »As far as we’re aware, the B.1.1 lineage originated from the B.1 lineage in China, from which it only differs in a few nucleotides«, explains Brandt. The numbers after the letter »B« indicate the mutation variants.
Doctoral candidate Mike Marquet, Dr Christian Brandt and Dr Oliwia Makarewicz (from right to left) from the Clinical Infectiology Research Laboratory at the Institute for Infectious Diseases and Infection Control carry out SARS-CoV-2 sequencing with the MinION system.
Image: Michael Szabó/UKJAccess for viruses denied
Bioinformaticians at Jena University Hospital (UKJ) are involved in a research project with the aim of finding molecular targets to prevent the coronavirus from multiplying and spreading in human cells. »That would effectively stop an infection«, says Prof. Rainer König from the research group »Systems Biology for Sepsis«. Prof. König is leading the sub-project at the UKJ. »The virus needs the reproductive mechanisms of host cells to replicate«. Similar to other viruses, SARS-CoV-2 enters cells of the host organism, where it is copied thousands of times before hijacking other cells and continuing to spread. The infected cells of the host don’t usually survive.
Prof. Rainer König
Image: Anne Günther (University of Jena)Instead of developing active ingredients to fight the rapidly changing virus proteins themselves, which could quickly lead to resistance, the research team is now trying to block the proteins of host cells in such a way that viruses are unable to use them. Well-researched examples are already available, such as the active ingredient sold under the name »Maraviroc«, which prevents HI viruses from entering immune cells by blocking the necessary receptor.
In the project, which has been allocated 500,000 euros funding by the Federal Ministry of Education and Research (BMBF), the consortium headed by Prof. König, Prof. Sandra Ciesek (University Hospital of Frankfurt am Main) and Dr Holger Erfle (University of Heidelberg) plans to down-regulate around 10,000 individual genes (host factors) for whose proteins inhibiting agents could be developed or already exist. The researchers are using high-throughput screening methods to observe whether tipping a host factor reduces or even stop virus replication and hence protects the host cells. For this, cells from a model human cell line (CaCo-2) are cultivated in microtiter plates and defined cell proteins are individually switched off. The researchers then try to infect the cells treated in this way with coronaviruses. By automatically taking microscopic images throughout the process, the researchers can ultimately observe the protective mechanism by this.
The images and data are then used for a cellular network analysis performed by Prof. König’s research group. »We’re using this information and other molecular data from publicly accessible databases to identify cellular processes that are essential for the virus’ lifecycle«. This may enable to identify compounds that most effectively disrupt the reproduction processes of SARS-CoV-2.
Proteins whose down-regulated genes demonstrate a protective effect (shown here schematically in red) are mapped onto a cellular network; repressor modules are defined (highlighted in red), and active ingredients are identified whose targets overlap with those modules (brown).
Graphic: Rainer König»We can’t hold our breath forever«
The motto at the beginning of the corona pandemic was »flatten the curve«. As in other countries, the federal and regional governments in Germany adopted extensive measures to slow down the momentum of the COVID-19 outbreak. »It was important to buy ourselves some time to adapt to the disease«, explains Dr Petra Dickmann de from the Anaesthesiology and Intensive Care unit at Jena University Hospital. The fact that the number of cases in Germany had fallen in the meantime shows that this strategy was correct. »However, measures like closing schools and social distancing are obviously not sustainable«, continues Dickmann. After all, we can’t »hold our breath« forever and have to return to public life. But just as we saw when public life was shut down in the first place, our policy-makers are now largely considering only short-term factors when easing the measures. »There are no rational criteria as to when and how certain measures can be eased without putting too much strain on the healthcare system«.
Billboard campaign in Jena during the Corona pandemic in March 2020.
Image: Anne Günther (University of Jena)These criteria are precisely what Petra Dickmann and her team want to develop with their colleagues in the »Pandemic Management« research group. The research group will receive around 480,000 euros in state funding by March 2021 to provide scientifically sound system of criteria that reflects the multiple dimensions of a pandemic.
The project has three pillars. Firstly, it aims to gain a better understanding of the infection burden; the research group has already developed an initial concept here: »We’ve proposed an early warning system that can be used to measure rate of infection, just like a movement detector«, says Petra Dickmann. Parts of a population should be tested for the coronavirus in a statistically reasonable sample size in relevant places, such as schools, nursing homes and care facilities, and in superspreading events. »We are looking at asymptomatic people that could carry the infection without symptoms and drive the outbreak.« The researchers adopt a strategic testing approach, that measures the infection rate in a community as a reflection of the entire population.
The second aim of the research project is to better understand the capacities of the healthcare system in the dynamic of demands. Hospitals have reserved intensive care beds and purchased additional ventilators to offer corona patients the best possible care. But how does this focus on COVID-19 affect the ability to care for all other patients? What examinations and treatments – from vaccination appointments and check-ups to chemotherapy – are currently taking place and how is the healthcare system equipped for such procedures? For this purpose, the research group has been working on an intensive care plan for the State of Thuringia.
And thirdly, Petra Dickmann and the working groups involved in the project are investigating the effects of the pandemic on the population. For example, they’re conducting a survey in cooperation with the COSMO Study at the University of ErfurtExternal link, where people are asked for their views on the pandemic and the preventive measures in Thuringia. Another focus of their research is risk communication in pandemic management, where the team is investigating the acceptance of quarantine measures and the information needs of affected people in quarantined areas as part of the »Neustadt Study«. Their findings are relevant to the current research and politics involved in pandemic management in Germany.
»Neustadt Study« – No antibodies in half of the infected subjects
At the beginning of March, the corona pandemic had also reached Thuringia. Once the first case of the novel virus had been confirmed on 2 March, the number of confirmed cases began to rise steadily. However, the hotspots of the outbreak in the Free State of Thuringia weren’t big cities like Erfurt or Jena, but places like Neustadt am Rennsteig – with a population of only 900 – where so many inhabitants became infected in such a short space of time that the whole place had to be quarantined for two weeks. By the end of the quarantine period, 49 corona cases had been confirmed by a mandatory screening of the entire population and two patients had died of COVID-19. Extrapolated to the population of the town, the figures were much higher than the regional average.
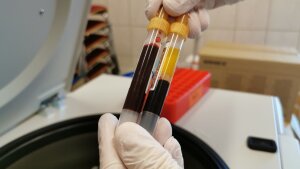
The blood samples of people from Neustadt am Rennsteig in Thuringia were examined at the JUH as part of the »Neustadt Study«. All residents of Neustadt were put in quarantine after several COVID-19 cases had been confirmed there.
Image: UKJ/HoppertAs in most towns and cities in Germany, the situation in Neustadt has now eased, giving researchers from Jena University Hospital the opportunity to take a closer look at the outbreak there. Prof. Mathias Pletz, the Director of the Institute of Infectious Diseases and Infection Control, is leading a team of ten researchers who are investigating the extent to which there might have been asymptomatic patients in addition to the 49 confirmed cases and whether those inhabitants of Neustadt have become immune to the virus. The researchers at the University of Jena have collected blood and pharyngeal wash samples from a total of 626 residents of all age groups – including young infants – of the town (71 percent of all inhabitants) and asked them about their symptoms during the illness and possible contact with the virus.
First results of the »Neustadt Study«pdf, 1 mb · de, which has been allocated 500,000 euros in funding from the Free State of Thuringia, are now available. Nobody in the town tested positive for SARS-CoV-2 at the time of the study. »We didn’t find any viruses circulating in the pharyngeal wash«, reports Dr Sebastian Weis, who was instrumental in the planning and execution of the study. In around 8 percent of the people examined, IgG antibodies were detected in at least two of six different COVID-19 antibody tests. »We did not find antibodies in about half of the study participants who had been confirmed to have the virus in March – although we had used several different tests«, said Prof Mathias Pletz. The researchers are now conducting further investigations to determine whether those people have developed special defence cells instead of antibodies. The results are expected over the course of the summer. Furthermore, the scientists also found antibodies in people who hadn’t been known to have contracted the virus. However, the results available so far aren’t enough to determine whether those individuals have built up an immunity to the virus.
In addition to the Institute of Infectious Diseases and Infection Control, four more institutes from the UKJ are involved in the study.
COVID-19 consultations at home
Four out of five patients infected with the novel coronavirus show a mild course of disease with symptoms similar to those of a heavy cold: fever, cough, headaches and aching limbs. »Those patients can usually cure the illness well at home«, says Dr Stefan Hagel from the Institute of Infectious Diseases and Infection Control at the Jena University Hospital. However, diagnostic monitoring from trained medical professionals is also important to identify a possible deterioration in the patient’s condition at an early stage and hospitalize them if necessary. After all, when a patient’s condition becomes critical, a quick response is of vital importance.
»But since patients are in quarantine at home, they can’t make it to their local doctor«, continues Dr Hagel. Furthermore, most doctors avoid home visits to COVID-19 patients to minimize the risk of spreading the virus even further. Many patients feel like they’ve been left to fight the disease on their own. However, a solution to this problem has now been established at Jena University Hospital, where a mobile app enables patients to monitor their own condition: The »MedoPad App« transmits diagnostic parameters (e.g. oxygen saturation of the blood, heart rate and body temperature) to the clinic several times a day, where doctors check the results to constantly monitor the progression of the disease.
COVID-19 patients can be monitored by taking oxygen measurements on their fingertip. A total of 400 pulse oximeter devices are available at the hospital and could be handed out to outpatients. The measurements are sent to the hospital via an app.
Image: Michael Szabó/UKJ»Our most important aim is to prevent severe developments«, explains Dr Hagel. Whenever patients develop pneumonia, their condition soon becomes critical and they’re often admitted to hospital too late. And that’s exactly what can be prevented through the monitoring app.
During the ongoing pilot phase, where the university hospitals in Jena and Heidelberg are working together thanks to an initiative launched by the Federal Ministry of Health (BMG), patients are given a pulse oximeter to take measurements three times a day. The data is transmitted straight to the hospital via the app. As soon as one or more values exceed or fall below a critical limit, the doctor contacts the patient to discuss the further treatment.
After using the MedoPad App for the past twelve weeks, Dr Hagel’s first impressions are very positive. However, the number of patients who have actually used the app to date is still manageable, as the number of cases in Jena and Thuringia is thankfully low. But the hospital is well prepared for a possible second wave of infections. A total of 400 pulse oximeter devices are available and could be handed out to outpatients.
Dr Stefan Hagel and Dr Aurelia Kimmig from the Institute of Infectious Diseases and Infection Con-trol at the UKJ are evaluating patient data transmitted via the MedoPad App.
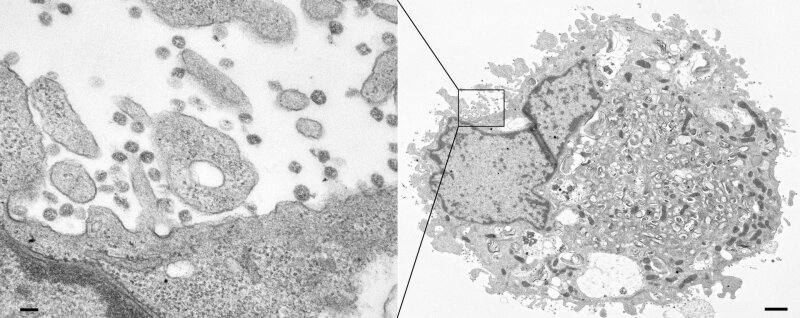
Image: Michael Szabó/UKJThis is what SARS-CoV-2 looks like
A team from the Electron Microscopy CentreExternal link at Jena University Hospital has succeeded in making SARS-CoV-2 visible. The electron micrograph shows numerous virus particles (dark circles in the left-hand image) exiting a cell after multiplying several times on the inside (right-hand image). The imaging was carried out using viruses cultivated from a COVID-19 patient treated at Jena University Hospital. The researchers now want to use the culture to investigate the replication of viruses within cells and their transmission from cell to cell.
Visualization of SARS-CoV-2 (dark circles in the left-hand image) taken using an electron micro-scope. Scale bar in the left-hand image: 100 nm; scale bar in the right-hand image: 1,000 nm (1 µm). For imaging purposes, the cells were treated with a contrast agent after the viral infection and then embedded in synthetic resin. Ultra-thin slices were then cut from the synthetic resin block (approx. 50 nm) and examined using a transmission electron microscope.
Picture: Dr. Sandor Nietzsche, Elektronenmikroskopisches Zentrum, Universitätsklinikum JenaBy Ute Schönfelder
More information and other COVID-19 research projects carried out at Jena University Hospital can be found here: https://www.uniklinikum-jena.de/Forschung/Covid_19_Forschung/Taskforce.htmlExternal link.